Healthier Australians
Shifting the dial article
18 January 2018
While on many measures, the Australian health system is very good compared with health care systems in many other countries, this is not true across the board. There is significant potential for improvement.
Australia has relatively high rates of chronic disease
While life expectancy has increased, Australians spend a relatively higher number of years in ill‑health, both in absolute terms and as a share of life expectancy. On both of these measures, Australia ranks second highest among a range of OECD and other developed countries.
Australians live longer, but a greater share of that life is spent in ill health compared with most countries, 2015
| Years spent in ill‑health as a share of life expectancy | Years of healthy life gained if Australia had the same ratio of ill‑health to life expectancy as Singapore |
|---|---|
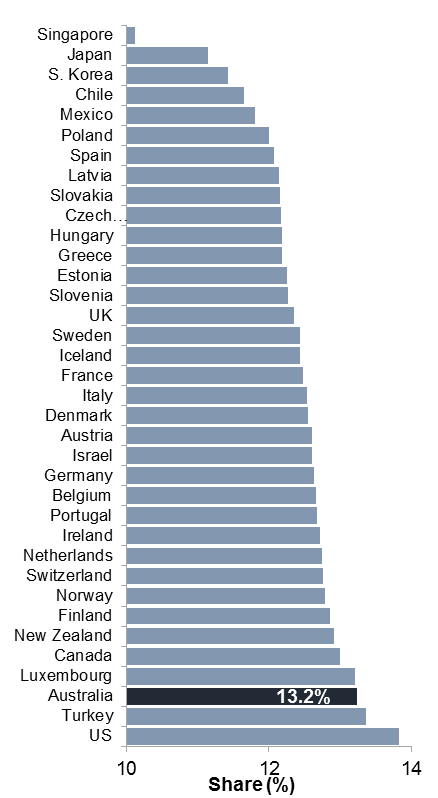
| 
|
Source: Institute for Health Metrics and Evaluation (IHME), 2016, Global Burden of Disease Study 2015.
As medical advances have lowered the rate of premature death from causes such as infectious disease and trauma, the focus of Australia’s health care system has shifted to managing chronic and complex conditions (such as diabetes, lung cancer, cardiovascular disease and mental illness). Nearly 45 per cent of Australians have three or more long‑term illnesses. Around three million people say they have only ‘fair to poor’ health. The ongoing nature of chronic conditions puts upward pressure on health care costs and inhibits people’s capacity to participate in society, including in the workforce.
The system has significant structural impediments
It is not patient centred
The patient experience receives little focus as a goal of the current system, which primarily responds to patient crisis. It is characterised by episodic treatment and medical procedures.
Services are fragmented
Care pathways, especially between primary and acute care (that is, between GPs and hospitals), are often poorly coordinated. Research indicates that less than 20 per cent of Australian GPs are informed when one of their patients is seen in a hospital emergency department. This compares with 68 per cent in the Netherlands, 56 per cent in New Zealand and 49 per cent in the United Kingdom.
Clinicians, patients and researchers are constrained by inadequate information flows and haphazard data collection. Private health insurance sits uneasily with a system of public insurance, with their respective roles weakly defined. Regulatory and jurisdictional obstacles prevent effective linkages between hospitals and GPs, which would enable better management of chronic conditions and reduce hospitalisations.
There are problems with quality
There is scope to improve safety and quality within the health care system. For example, hospital-acquired complications and avoidable hospital readmissions have not significantly decreased in recent years. Many medical interventions, funded by taxpayers, are undertaken despite little evidence that the intervention is beneficial (arthroscopic knee surgery is a case in point) There is evidence that GPs could play a greater role in preventing chronic conditions. The Australasian College of General Practice has emphasised SNAP — smoking, nutrition, alcohol and physical activity — as key targets for preventative care. Yet most people in the SNAP categories have not had discussions with their GPs about preventative health. And health outcomes are poorer for low-income households, non-metropolitan regions and Indigenous Australians.
The solution: integrated, patient-centred care
The Commission recommends reforms aimed at achieving integrated, patient-centred health care, delivering customised services to people across the entire health system. The aim is to improve health outcomes, while delivering a higher quality, more cost-effective service to patients.
Some of the ingredients are already present, and some parties in the system try to integrate services — by developing care plans, communicating with other clinicians and allied health professionals, and following up on hospital admissions — but are frequently frustrated by the structural barriers within the system, such as incompatible information systems, weak linkages between the various health professionals, gaps in availability of services, and funding models which discourage integration.
Patient-centred care involves ‘clinical redesign’ to manage the patient journey through the system. It treats the person as the central party around whom resources and processes that improve their wellbeing are assembled. All aspects of health service delivery are coordinated to provide quality outcomes at minimum cost to match the different preferences and needs of all customers.
While an integrated system of patient‑centred health care has been a policy objective in all Australian jurisdictions since a COAG agreement in 1995, progress towards a genuine Australia‑wide integrated system across all health care sectors has been poor.
Integrated, patient‑centred health care requires complex inter‑linked policy initiatives to make it work
A patient‑centred health system revolves around the patient, giving them agency through choice, shared decision making with medical professionals, and the capacity for self‑management (where feasible). It is premised on the expectation that people will take some responsibility for their own health.
This requires:
- Acceptance of the principle that patients are the centre of the system by all actors in the health care system (in the same way that disability care has shifted). Many Australian governments have accepted this premise, but patient‑centredness requires structural reforms and attitudinal changes by clinicians and patients.
- Raising people’s health literacy (the capacity to understand information about their health and the factors that impinge on it). This means providing information that allows patients to be participants in their care, including, where feasible, the capacity to exercise choice. This will involve:
- rights to patient data, including through an enhanced role for My Health Record
- provision of information on system performance (including new measures of the performance of clinicians, hospitals and other organisations), transparency of prices, and indicators of the quality of services provided by hospitals and clinicians.
For more discussion about how to improve health literacy, including performance measures for hospitals and clinicians, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 3
Regional flexibility is critical
Health care needs vary across regions, reflecting variations in the characteristics of regional populations and differences in local knowledge and relationships. Integration of health care services is generally best managed at a regional level, which provides an efficient scale for managing health service delivery and integration. It also allows for flexibility in meeting the specific needs of individual regions.
All jurisdictions have made progress towards a regional approach to care. Local Hospital Networks (LHN) are public sector bodies that manage hospitals and state government health services in a given area. Primary Health Networks (PHN) are private entities that have been contracted by the Australian Government to improve the efficiency and effectiveness of services and to coordinate patient care in their locality, including by working collaboratively with Local Hospital Networks. Some PHNs and LHNs have been building on this foundation, working together to deliver integrated health — and where they do, for example in Western Sydney, Brisbane North, and the Hunter, they are proving effective for improving the coordination of care However, the journey is far from complete, nor the arguments for it, completely accepted.
For more discussion about developing a regional model of integrated care, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 4
Funding models should encourage integration across the system
A drawback of Australia’s current health system is that there are a series of budget silos. Hospitals are managed by State and Territory Governments, and jointly funded by both levels of government; general practice is funded and regulated by the Australian Government; and community health care centres are funded and managed by State and Territory Governments. Key decision makers in our system have no direct financial incentive to be efficient in their use of other parts of the system.
In a well‑integrated system, there would be incentives for health care providers to direct people to the most suitable and cost effective services, and where possible, prevent the onset of chronic conditions. Achieving that outcome is not straightforward.
Activity‑based funding of hospitals has improved efficiency, but only within hospitals
Major Australian hospitals are funded for the bulk of their services through activity based funding (ABF), under which they receive revenues based on the efficient costs of delivering specified services to their mix of patients. Following the introduction of ABF, national growth in the average cost of providing hospital services has slowed significantly.
Fee‑for‑service does not encourage fully‑integrated care
GPs and specialists are generally paid on a fee‑for‑service basis for items on the government‑determined Medicare Benefits Schedule (MBS). This means clinicians do not face strong financial incentives to avoid high‑cost activities (such as tests, referrals to specialists, and hospital admissions), use lower‑cost delivery methods (such as employing nurse practitioners or phone‑based consultations), or encourage coordinated care of patients or disease management. Moreover, fee‑for‑service introduces considerable rigidity into the management of care.
While Australia’s health system has many positive attributes, there are significant limitations in its funding models and service structures, including the lack of incentives for different sectors to cooperate and efficiently provide integrated services across hospitals, general practice and community care.
Changes to hospital funding
Hospital funding should be re-designed to create incentives to cost‑effectively avoid hospitalisations through investments in public health and in community and primary care. The Commission proposes an approach whereby LHNs are able to make investments outside a hospital setting (such as commissioning the services of GPs) to reduce more costly hospitalisations, with the overall outcome being a fall in hospital costs currently funded through ABF, but with LHNs obtaining a share of the savings.
One way to enable this would be to establish a Prevention and Chronic Condition Management Fund (PCCMF) in each local health district. The LHN in each district would decide how and where to spend funds from the PCCMF, often in collaboration with other local partners. There should be few restrictions on the types of investments made by LHNs. For instance, if low‑cost community initiatives to reduce loneliness among older people reduced hospitalisations, then this would be an attractive intervention. So too might an alliance with PHNs that led to more effective management of people with incipient obesity, and thereby, at some later time, reduced rates of type 2 diabetes, and lower hospitalisation rates.
For more discussion about the Commission’s proposed reforms to hospital funding, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 6
Changes to primary care funding
The Commission proposes the implementation of a ‘blended payments’ model for GPs, retaining fee-for-service as a major portion of GP revenue, combined with risk-adjusted capitation payments. This would strengthen incentives for GPs to provide services via multidisciplinary teams, including a greater role in preventative health and management of chronic conditions.
More flexible funding pools and partnerships at the regional level are needed to give general practice and other health professions scope to adopt more innovative models of care. LHNs should be given capacity to fund GPs to work with hospitals to better manage the care of patients with complex and chronic conditions.
Under a regionally-based integrated care model, MBS funding would continue, but its role would generally diminish as PHNs and LHNs developed other ways to remunerate GPs for clinical outcomes, or processes linked to good outcomes.
For more discussion about the Commission’s proposed reforms to primary care funding, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 6
Financial incentives for improving quality and safety should not be overlooked
Despite some recent tightening, hospitals can still receive funding for many preventable events (such as hospital‑acquired complications (HACs) and avoidable hospital readmissions). Unplanned readmissions have shown little downward trend in recent years, and there are significant variations between hospitals, suggesting inadequate diffusion of best practice.
Unplanned readmissions for 6 surgical procedures
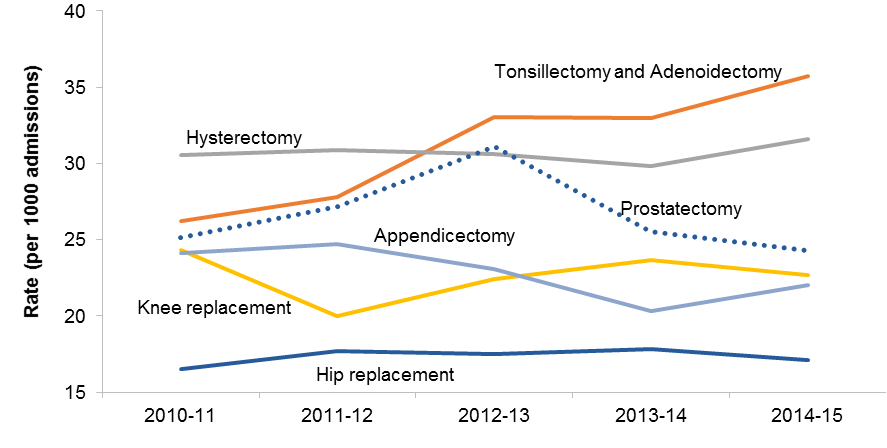
a An unplanned readmission occurs where a patient is admitted for an unplanned care or service in a hospital within 28 days of an earlier discharge. Not all unplanned readmissions are necessarily avoidable, but they are recognised as a valid indicator of safety and quality in State and Territory Government Service Performance Agreements with LHNs. The data are limited to public hospitals. Only the first readmission following surgery was included. A readmission was not included if there was an intervening unrelated separation.
Source: SCRGSP (2017 table 12A.50).
There has been limited national progress in reducing medical interventions for which there is little or no evidence of benefits, suggesting problems in patient awareness and dissemination of evidence-based medicine across clinicians.
To overcome these problems, the Commission concludes that, amongst other things, Australian governments should:
- more quickly respond to authoritative assessments identifying low-value interventions, and de-fund interventions that fail cost-effectiveness tests.
- collect and divulge data at the hospital and clinician level for episodes of care that lead to hospital acquired complications and for interventions that have ambiguous clinical impacts.
- provide patients with plain English explanations of treatments that often lack efficacy.
Rate of knee anthroscopy hospital admissions
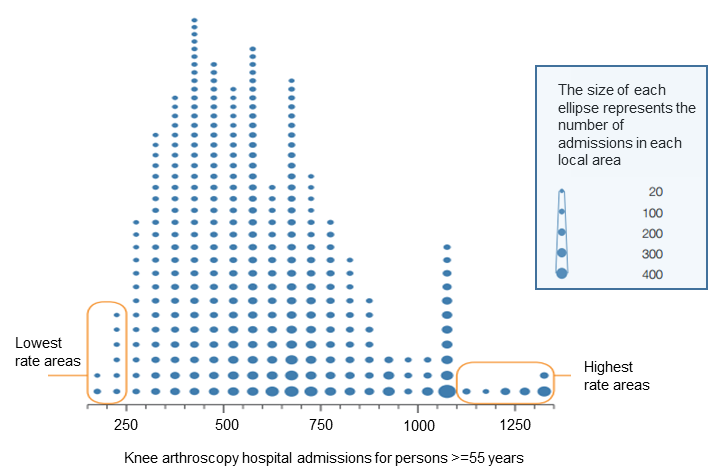
a The local area refers to the ABS Statistical Area Level 3 classification of geographic regions.
Source: ACSQHC 2015, Australian Atlas of Healthcare Variation, chapter 3.1 (p. 107).
For more discussion about improving quality and safety of Australia’s health care system, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 7
Better data collection and information sharing
Integrated and effective data and information systems are a critical element of an integrated system of care. Information technology provides the capacity to collect, link, analyse, aggregate and store vast amounts of data on what is done to patients, who does it, billing, the performance of health providers, and to some degree, the outcomes for people of health interventions. IT also has the capacity to empower patients by giving them information about their own health and the performance of the clinicians and providers with whom they interact. Data can revolutionise research into ‘what works’.
However, seamless information sharing across the Australian health system has failed to materialize. The OECD has characterised Australia as relatively poor in its capacity to collect and link data. While a huge amount of data are collected, there are substantial gaps, a lack of integration and sporadic use.
Poor information flows raise the risks of conflicting treatments, duplication of effort, suboptimal outcomes, inconvenience for patients, and excessive costs.
The Commission has undertaken an extensive inquiry into Data Availability and Use (released in 2017), which sets out a comprehensive suite of policies that make data a useful asset — not just in health, but across the economy. That inquiry provides the roadmap for reform, including the need for more open data, and protocols that would allow the data to be linked and used for the public good, while addressing privacy concerns.
For more discussion about how data collection and management can be improved in the Australian health care system, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 9
Transitioning to a new system
While the shift to integrated care has been slow and disjointed, Australia’s health system is now much more coordinated than in the past. All Australian governments have implemented — if sometimes only on a trial basis — various forms of integrated care. And there is increasing support from clinicians about the desirability of adopting integrated care as the basis of the Australian health care system.
Although not fully joined up yet, some of the key ingredients of an Australia‑wide integrated care system are in place, including:
- community health care centres throughout Australia
- bodies that play a role in coordinating or managing services at the regional level (PHNs and LHNs)
- greater use of telehealth
- more sophisticated national approaches to funding all public hospitals through activity‑based funding
- the emerging development of patient experience indicators
- national institutions that aim to ensure safety and quality in health care services
- an awareness of the power of data, and the growing development of systems that allow its exploitation
- a nationwide approach to organ donations
- the rollout of My Health Record
However, progress towards a patient-centered approach in primary care remains slow.
For a summary of the critical issues required to ensure the successful transition to an integrated, patient-centred health care system, see Shifting the Dial: 5 Year Productivity Review. Supporting Paper 5, Chapter 10, Table 10.1
Health
- More than 10 million Australians have three or more long-term conditions (SP4, p. 10)
- Years of life spent in ill-health are nearly 11 years — highest in the OECD (p. 45)
- 4.9 million adults (nearly 30% of the adult population) are obese (p. 45)
- 11.7 million people have no or low exercise levels (2 in 3 adults) ( p. 45)
- Moving from poor health to fair health increases labour participation rates by 34 percentage points (SP4. p. 14)
- 75% of acute bronchitis is treated with antibiotics. The appropriate rate is close to zero (p. 61)
- Unnecessary waiting in doctor’s rooms costs Australians around $1 billion annually in lost time (p. 64)
- 40% of people with a health-related qualification have inadequate health literacy (p. 65)
A full list of the Commission’s recommendations, including implementation strategies for each recommendation, are contained in the main report Shifting the Dial: 5 Year Productivity Review, available at: www.pc.gov.au/inquiries/completed/productivity-review/report