Report on Government Services 2022
PART E, SECTION 13: RELEASED ON 1 FEBRUARY 2022
13 Services for mental health
Impact of COVID-19 on data for the Services for mental health section
COVID-19 may affect data in this report in a number of ways. This includes in respect of actual performance (that is, the impact of COVID-19 on service delivery during 2020 and 2021 which is reflected in the data results), and the collection and processing of data (that is, the ability of data providers to undertake data collection and process results for inclusion in the report).
For the Services for mental health section, there has been some impact on the data that is attributable to COVID-19. In 2019-20 and 2020-21, a range of new items relating to the provision of health care via telehealth and additional individual psychology sessions were added to the Medicare Benefits Schedule (MBS). COVID-19 also affected data collection and results for several performance indicators. The ABS General Social Survey ceased face-to-face interviewing and that combined with the impact of COVID-19 restrictions during the survey period means care should be taken when interpreting the 2020 data for social inclusion and stigma and discrimination. Victoria did not participate in the Your Experience of Service (YES) survey during 2019-20 due to the COVID-19 pandemic which affects the available data for consumer experiences of mental health services.
This section reports on the Australian, State and Territory governments’ management of mental health and mental illnesses. Performance reporting focuses on State and Territory governments’ specialised mental health services, and services for mental health subsidised under the Medicare Benefits Schedule (MBS) (provided by General Practitioners (GPs), psychiatrists, psychologists and other allied health professionals).
The Indicator Results tab uses data from the data tables to provide information on the performance for each indicator in the Indicator Framework. The same data are also available in CSV format.
- Context
- Indicator framework
- Indicator results
- Indigenous data
- Key terms and references
Objectives for services for mental health
Services for mental health aim to:
- promote mental health and wellbeing, and where possible prevent the development of mental health problems, mental illness and suicide, and
- when mental health problems and illness do occur, reduce the impact (including the effects of stigma and discrimination), promote recovery and physical health and encourage meaningful participation in society, by providing services that:
- are high quality, safe and responsive to consumer and carer goals
- facilitate early detection of mental health issues and mental illness, followed by appropriate intervention
- are coordinated and provide continuity of care
- are timely, affordable and readily available to those who need them
- are sustainable.
Governments aim for services for mental health to meet these objectives in an equitable and efficient manner.
Service overview
Mental health relates to an individual’s ability to negotiate the daily challenges and social interactions of life without experiencing undue emotional or behavioural incapacity (DHAC 1999). The World Health Organization describes positive mental health as:
… a state of wellbeing in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community (WHO 2001).
Mental illness is a term that describes a diverse range of behavioural and psychological conditions. These conditions can affect an individual’s mental health, functioning and quality of life. Each mental illness is unique in its incidence across the lifespan, causal factors and treatments.
There are a range of services provided or funded by Australian, State and Territory governments that are specifically designed to meet the needs of people with mental health issues; the key services are:
- MBS subsidised mental health specific services that are partially or fully funded under Medicare on a fee-for-service basis and are provided by GPs, psychiatrists, psychologists or other allied health professionals under specific mental health items.
- State and Territory government specialised mental health services (treating mostly low prevalence, but severe, mental illnesses), which include:
- Admitted patient care in public hospitals — specialised services provided to inpatients in stand-alone psychiatric hospitals or psychiatric units in general acute hospitals1.
- Community-based public mental health services, comprising:
- ambulatory care services and other services dedicated to assessment, treatment, rehabilitation and care, and
- residential services that provide beds in the community, staffed onsite by mental health professionals.
- Not for profit, non-government organisation (NGO) services, funded by the Australian, State and Territory governments focused on providing wellbeing, support and assistance to people who live with a mental illness. These include crisis, support and information services such as Beyond Blue, Lifeline, Kids Helpline, and ReachOut.
- The National Disability Insurance Scheme (NDIS), which began full roll out in July 20162. People with a psychiatric disability who have significant and permanent functional impairment are eligible to access funding through the NDIS. In addition, people with a disability other than a psychiatric disability, may also be eligible for funding for mental health-related services and support if required.
- Whilst not a State and Territory government specialised mental health service, this section also reports on emergency department presentations for mental health related care needs (where data are available). Locate Footnote 1 above
- For further information on the NDIS and its implementation see https://www.ndis.gov.au/. Locate Footnote 2 above
Roles and responsibilities
State and Territory governments are responsible for the funding, delivery and/or management of specialised services for mental health including inpatient/admitted care in hospitals, community-based ambulatory care and community-based residential care.
The Australian Government is responsible for the oversight and funding of a range of services for mental health and programs that are primarily provided or delivered by private practitioners or NGOs. These services and programs include MBS subsidised services provided by GPs (under both general and specific mental health items), private psychiatrists and other allied mental health professionals, Pharmaceutical Benefits Scheme (PBS) funded mental health-related medications and other programs designed to prevent suicide or increase the level of social support and community-based care for people with a mental illness and their carers. The Australian Government also funds State and Territory governments for health services, most recently through the approaches specified in the National Health Reform Agreement (NHRA) which includes a mental health component.
A number of national initiatives and nationally agreed strategies and plans underpin the delivery and monitoring of services for mental health in Australia including:
- the Mental Health Statement of Rights and Responsibilities (Australian Health Ministers 1991)
- the National Mental Health Policy 2008 (DoH 2009)
- the National Mental Health Strategy (DoH 2014)
- five-yearly National Mental Health Plans, with the most recent ― the Fifth National Mental Health and Suicide Prevention Plan — endorsed in August 2017 (COAG 2017).
Funding
Nationally, real government recurrent expenditure of around $10.4 billion was allocated to services for mental health in 2019‑20, equivalent to $408.81per person in the population (table 13A.1 and figure 13.1). State and Territory governments made the largest contribution ($6.6 billion or 63.3 per cent, which includes Australian Government funding under the NHRA), with Australian Government expenditure of $3.8 billion (table 13A.2).
Expenditure on MBS subsidised services was the largest component of Australian Government expenditure on services for mental health in 2019‑20 ($1.4 billion or 37.2 per cent) (table 13A.2). This comprised MBS payments for psychologists and other allied health professionals (17.8 per cent), consultant psychiatrists (10.7 per cent) and GP services (8.7 per cent) (table 13A.2). Another significant area of Australian Government expenditure on services for mental health in 2019‑20 was expenditure under the PBS for mental health-related medications ($551.0 million) (table 13A.2).
Nationally, expenditure on admitted patient services is the largest component of State and Territory governments’ expenditure on specialised mental health services ($2.9 billion or 43.6 per cent) in 2019‑20 followed by expenditure on community-based ambulatory services ($2.6 billion or 36.6 per cent) (table 13A.3). State and Territory governments’ expenditure on specialised mental health services, by source of funds and depreciation (which is excluded from reporting) are in tables 13A.4 and 13A.5 respectively.
Size and scope
In 2020-21, 11.6 per cent of the total population received MBS/DVA services, with 1.9 per cent of the total population receiving State/Territory governments’ specialised mental health services in 2019-20 (the most recent of data available) (figure 13.2). While the proportion of the population using State and Territory governments’ specialised mental health services has remained relatively constant, the proportion using MBS/DVA services has increased steadily over time from 7.3 per cent in 2011-12 to 11.6 per cent in 2020‑21 (table 13A.7). Much of this growth has come from greater utilisation of GP mental health-specific services (from 5.7 per cent to 9.6 per cent) and other allied health services (2.3 per cent to 3.6 per cent) over that period (table 13A.7).
Information on the proportion of new consumers who accessed State and Territory governments’ specialised and MBS subsidised services for mental health are available in tables 13A.8–9.
MBS subsidised services for mental health
In 2020‑21, 9.9 million MBS subsidised services for mental health were provided by; psychologists (clinical and other services) (6.6 million), psychiatrists (2.7 million) and other allied health professionals (0.6 million). Service usage rates varied across states and territories (table 13A.10).
A further 4.1 million MBS subsidised specific services for mental health were provided by GPs (table 13A.10). GPs are often the first service accessed by people seeking help when suffering from a mental illness (AIHW 2021). They can diagnose, manage and treat mental illnesses and refer patients to more specialised service providers. A 2019 report from the Royal Australian College of General Practitioners found that mental health issues are the most common single reason patients are visiting their GP (RACGP 2019). Data from the now decommissioned Bettering the Evaluation and Care of Health (BEACH) survey of general practice activity showed an estimated 18.0 million GP visits in 2016‑17 included management of mental health related problems (12.4 per cent of all GP encounters) (table 13A.11).
State and Territory governments’ specialised mental health services
Across states and territories, the mix of admitted patient and community-based services and care types can differ. As the unit of activity varies across these three service types, service mix differences can be partly understood by considering items which have comparable measurement such as expenditure (table 13A.3), numbers of full time equivalent (FTE) direct care staff (table 13A.12), accrued mental health patient days (table 13A.13) and mental health beds (table 13A.14).
Additional data are also available on the most common principal diagnosis for admitted patients, community-based ambulatory contacts by age group and specialised mental health care by Indigenous status in Mental Health Services in Australia (AIHW 2021).
Crisis and support organisations
Crisis, support and information services such as Beyond Blue, Lifeline, Kids Helpline, and ReachOut are provided to support Australians experiencing mental health issues. In 2020-21:
- Lifeline had almost 1.1 million calls offered
- Kids Helpline received around 349 230 answerable contacts attempts (call, webchat and email)
- 315 217 contacts were made to Beyond Blue (call, webchat and email) (AIHW 2021).
National Disability Insurance Scheme
The National Disability Insurance Scheme (NDIS) provides support to people with a significant and enduring primary psychosocial disability. In 2020-21, there were 48 458 NDIS participants (active with an approved plan) with a psychosocial disability (10.0 per cent of all participants) (NDIA 2021).
Nationally in 2020‑21, payments for active participants (with an approved plan) for people with a primary disability of psychosocial disability totalled $2.2 billion (table 13A.15).
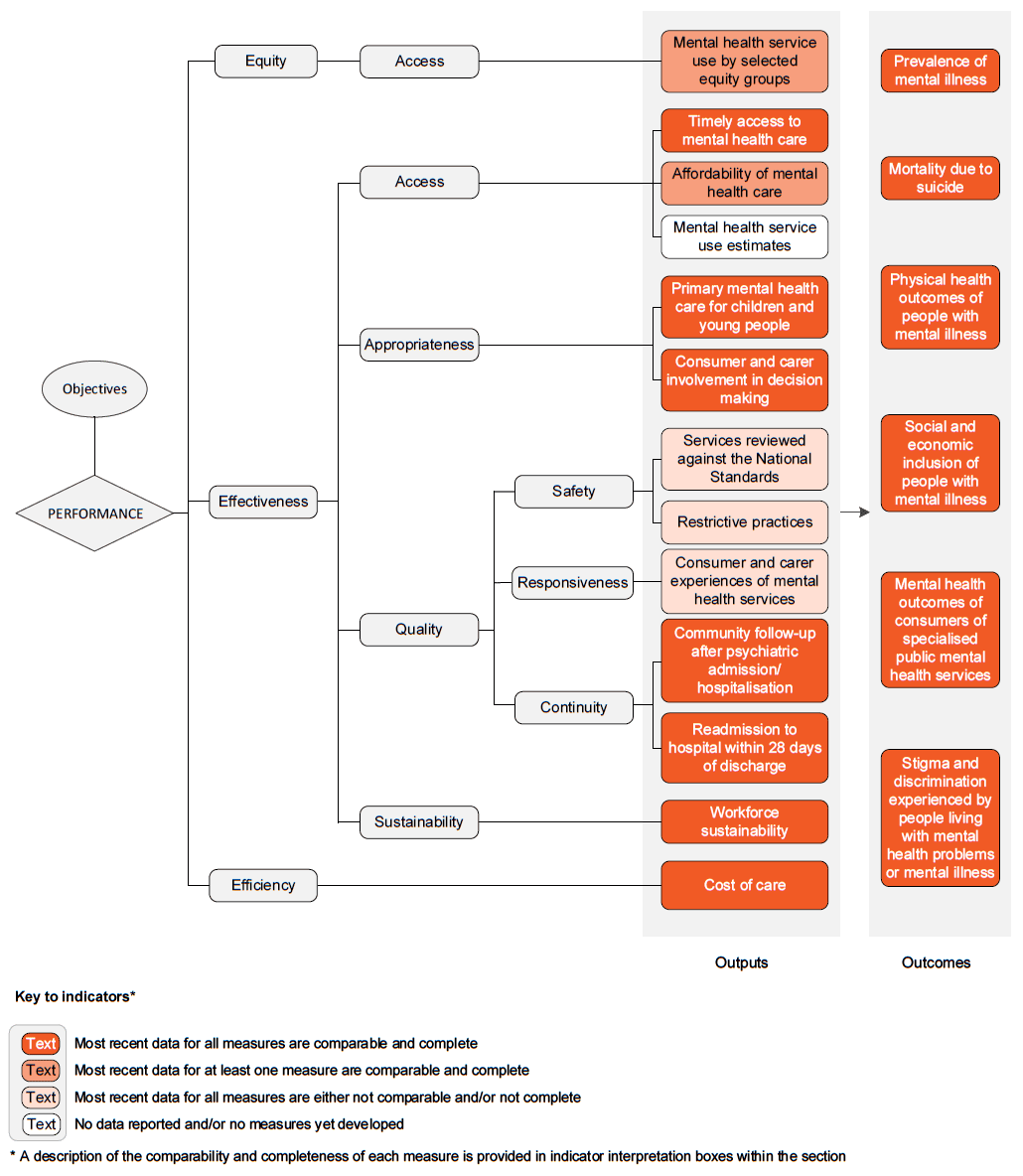
The performance indicator framework provides information on equity, efficiency and effectiveness, and distinguishes the outputs and outcomes of services for mental health.
The performance indicator framework shows which data are complete and comparable in this Report. For data that are not considered directly comparable, text includes relevant caveats and supporting commentary. Section 1 discusses data comparability and completeness from a Report-wide perspective. In addition to the contextual information for this service area (see Context tab), the Report’s statistical context (section 2) contains data that may assist in interpreting the performance indicators presented in this section.
Improvements to performance reporting for services for mental health are ongoing and include identifying data sources to fill gaps in reporting for performance indicators and measures, and improving the comparability and completeness of data.
Outputs
Outputs are the services delivered (while outcomes are the impact of these services on the status of an individual or group) (see section 1). Output information is also critical for equitable, efficient and effective management of government services.
Outcomes
Outcomes are the impact of services on the status of an individual or group (see section 1).
An overview of the Services for mental health performance indicator results are presented. Different delivery contexts, locations and types of consumers can affect the equity, effectiveness and efficiency of services for mental health.
Information to assist the interpretation of these data can be found with the indicators below and all data (footnotes and data sources) are available for download from Download supporting material. Data tables are identified by a ‘13A’ prefix (for example, table 13A.1).
All data are available for download as an excel spreadsheet and as a CSV dataset — refer to Download supporting material. Specific data used in figures can be downloaded by clicking in the figure area, navigating to the bottom of the visualisation to the grey toolbar, clicking on the 'Download' icon and selecting 'Data' from the menu. Selecting 'PDF' or 'Powerpoint' from the 'Download' menu will download a static view of the performance indicator results.
1. Mental health service use by selected equity groups
‘Mental health service use by selected equity groups’ is an indicator of governments’ objective to provide services in an equitable manner.
‘Mental health service use by selected equity groups’ is defined by two measures:
- the proportion of the population in a selected equity group using the service, compared to the proportion of the population outside the selected equity group, for each of:
- State and Territory governments’ specialised public mental health services
- MBS/ DVA subsidised mental health services.
The selected equity groups reported are Aboriginal and Torres Strait Islander people, people from outer regional, remote and very remote locations and people residing in low socioeconomic areas (Socio Economic Indexes for Areas (SEIFA) quintiles 1 and 2).
Results for this indicator should be interpreted with caution. Variations in use could be due to variations in access, but could also be a result of differences in the prevalence of mental illness. It also does not provide information on whether the services are appropriate for the needs of the people receiving them, or correctly targeted to those most in need.
While a higher proportion of the population access MBS/DVA subsidised mental health services than State and Territory governments’ specialised public mental health services (table 13A.7), the pattern of service use across the selected equity groups differs.
In 2019-20, for State and Territory governments’ specialised public mental health services, a higher proportion of Aboriginal and Torres Strait Islander people access these services than non-Indigenous people (figure 13.3). People residing in lower socioeconomic areas (SEIFA quintiles 1 and 2) have greater usage of mental health services compared to people residing in higher socioeconomic areas (SEIFA quintiles 4 and 5) and people in outer regional, remote and very remote areas have greater usage usage compared to other areas.
Nationally in 2020-21, the proportion of people who accessed MBS/DVA services was lower for people in lower socioeconomic areas compared to higher socioeconomic areas and lower for people in outer regional, remote and very remote areas compared to other areas, though results varied across jurisdictions.
Data on the use of private hospital mental health services are also contained in tables 13A.16–18 and 13A.7.
2. Timely access to mental health care
‘Timely access to mental health care’ is an indicator of governments’ objective to provide services in a timely manner.
‘Timely access to mental health care’ is defined as the proportion of people who present to an emergency department with a mental health related care need (principal diagnosis of F00–F99) seen within clinically recommended waiting times.
The proportion of people seen within clinically recommended waiting times is defined as the proportion of patients seen within the benchmarks set by the Australasian Triage Scale. The Australasian Triage Scale is a scale for rating clinical urgency, designed for use in hospital-based emergency services in Australia and New Zealand. The benchmarks, set according to triage category, are as follows:
- triage category 1: need for resuscitation — patients seen immediately
- triage category 2: emergency — patients seen within 10 minutes
- triage category 3: urgent — patients seen within 30 minutes
- triage category 4: semi urgent — patients seen within 60 minutes
- triage category 5: non urgent — patients seen within 120 minutes.
High or increasing proportions of patients seen within the recommended waiting times is desirable. Contextual data for all presentations (not just those with a mental health related care need) are reported in section 12.
This is a partial measure for this indicator as emergency departments are only one of many services that provide access to mental health care. Future reporting will focus on timely access to State and Territory governments’ specialised public mental health services and MBS subsidised services for mental health.
Nationally in 2019-20, 68.0 per cent of people who presented to an emergency department with a mental health related care need were seen within clinically recommended waiting times (figure 13.4).
3. Affordability of mental health care
‘Affordability of mental health care’ is an indicator of governments’ objective to provide services that are affordable.
‘Affordability of mental health care’ is defined by three measures:
- The proportion of people who delayed seeing or did not see a GP for their mental health due to cost
- The proportion of people who delayed seeing or did not see a psychologist, psychiatrist or other mental health professional for their mental health due to cost
- The proportion of people who delayed filling or did not fill a prescription for their mental health due to cost
A low or decreasing proportion for each measure is desirable.
In 2020-21, the proportion of people who delayed or did not see a psychologist, psychiatrist or other mental health professional for their mental health due to cost was higher than those who delayed or did not see a GP for their mental health due to cost (15.3 and 5.8 per cent respectively) (figure 13.5).
4. Mental health service use estimates
‘Mental health service use estimates’ is an indicator of governments’ objective to provide services that are readily available to those who need them.
‘Mental health service use estimates’ is defined as the estimated proportion of the population with a mental health condition receiving a mental health service.
A high or increasing proportion of the population with a mental health condition receiving services for mental health suggests greater access to treatment. However, not all people with a mental health condition will want or need treatment. Furthermore, accessing a service does not guarantee that the service will be effective.
An agreed method for reporting against this indicator is not yet available.
5. Primary mental health care for children and young people
‘Primary mental health care for children and young people’ is an indicator of governments’ objective to facilitate early detection of mental health issues and mental illness, followed by appropriate intervention.
‘Primary mental health care for children and young people’ is defined as the proportion of young people aged under 25 years who received a mental health care service subsidised through the MBS from a GP, psychologist or other allied health professional.
High or increasing proportions of young people who had contact with MBS subsidised primary mental health care services are desirable.
Results for this indicator should be interpreted with caution. Variations in use could be due to variations in access, but could also be a result of differences in the prevalence of mental illness. In addition, this indicator does not provide information on whether the services are appropriate for the needs of the young people receiving them, or correctly targeted to those young people most in need. Further, some primary mental health services for children and young people are excluded from these data; for example, community health centres, school and university counsellors and health nurses and some mental health care provided by State and Territory governments’ specialised mental health services (NMHPSC 2011a).
The proportion of all children and young people who receive MBS subsidised primary mental health care services has doubled over the past 10 years, from 4.9 per cent in 2011-12 to 10.3 per cent in 2020-21. The proportion increases as age increases; with the highest proportion for young people aged 18–24 years (17.2 per cent nationally in 2020-21 ) (figure 13.6).
Proportions are higher for females compared to males, and for major cities and inner regional areas compared to other areas (table 13A.22). Data by Indigenous status and service type are available in tables 13A.22–23 respectively.
6. Consumer and carer involvement in decision making
‘Consumer and carer involvement in decision making’ is an indicator of governments’ objective to provide universal access to services that are responsive to consumer and carer goals.
‘Consumer and carer involvement in decision making’ is defined by two measures, the number of paid FTE:
- consumer workers per 1000 FTE direct care staff
- carer workers per 1000 FTE direct care staff.
High or increasing proportions of paid FTE direct care staff who are consumer or carer workers implies better opportunities for consumers and carers to influence the services received.
Nationally in 2019-20, there were:
- 7.0 paid FTE consumer workers per 1000 paid FTE direct care staff (figure 13.7a)
- 2.5 paid FTE carer workers per 1000 paid FTE direct care staff (figure 13.7b).
7. Services reviewed against the National Standards
‘Services reviewed against the National Standards’ is an indicator of governments’ objective to provide universal access to services that are high quality.
‘Services reviewed against the National Standards’ is defined as the proportion of expenditure on State and Territory governments’ specialised public mental health services that had completed a review by an external accreditation agency against the National Standards for Mental Health Services (NSMHS) and met ‘all standards’ (level 1). The assessment levels are defined in the ‘Key terms and references’ tab.
A high or increasing proportion of expenditure on specialised mental health services that had completed a review by an external accreditation agency and had been assessed against the NSMHS as level 1 is desirable.
This is a process indicator of quality, reflecting progress made in meeting the NSMHS. It does not provide information on whether the standards or assessment process are appropriate. In addition, services that had not been assessed do not necessarily deliver services of lower quality. Some services that had not completed an external review included those that were undergoing a review and those that had booked for review and were engaged in self-assessment preparation.
Nationally, as at 30 June 2020, 88.0 per cent of expenditure on specialised public mental health services that had completed an external review against the NSMHS was on services that met ‘all standards’ (level 1) (figure 13.8).
8. Restrictive practices
‘Restrictive practices’ is an indicator of governments’ objective to provide access to services that are safe.
‘Restrictive practices’ is defined by two measures:
- ‘Seclusion rate’, defined as the number of seclusion events per 1000 bed days in State and Territory governments’ specialised mental health acute inpatient units
- ‘Restraint rate’, defined by two sub measures:
- the number of mechanical restraint events per 1000 bed days in State and Territory governments’ specialised mental health acute inpatient units
- the number of physical restraint events per 1000 bed days in State and Territory governments’ specialised mental health acute inpatient units.
Seclusion involves a patient being confined at any time of the day or night alone in a room or area from which he or she cannot leave (the ‘Key terms and references’ tab provides further details on seclusion and ‘seclusion events’). Legislation or mandatory policy governs the use of seclusion in each State and Territory and may result in exceptions to the definition of a seclusion event and variations in the data collected across jurisdictions (NMHPSC 2011b).
Restraint is defined as the restriction of an individual’s freedom of movement by physical or mechanical means. The ‘Key terms and references’ tab provides further details on mechanical and physical restraint.
A low or decreasing number of seclusion and restraint events per 1000 bed days in specialised public mental health inpatient units is desirable.
Supporting data on the duration of seclusion events are provided in table 13A.26. These data, when considered with the rate of seclusion, provide information on the use and management of seclusion within each jurisdiction. A low rate of seclusion events combined with shorter average durations is desirable.
Nationally (excluding Tasmania) in 2020-21, the rate of seclusion was 7.3 events per 1000 bed days (figure 13.9a).
Nationally (excluding Tasmania) in 2020-21, the rate of physical restraint was 11.6 events per 1000 bed days, and for mechanical restraint was 0.7 events per 1000 bed days (figure 13.9b and table 13A.28).
For both seclusion and restraint, results varied across target populations (tables 13A.27 and 13A.29). In 2020-21, the lowest seclusion, physical and mechanical restraint rates were in Older persons units and the highest were in Forensic units (tables 13A.27 and 13A.29).
9. Consumer and carer experiences of mental health services
‘Consumer and carer experiences of mental health services’ is an indicator of governments’ objective to provide access to services that are responsive to consumer and carer goals.
‘Consumer and carer experiences of mental health services’ is defined by two measures:
- the proportion of mental health service consumers reporting positive experiences of mental health services
- the proportion of carers of mental health service consumers reporting positive experiences of mental health services
A high or increasing proportion of mental health consumers and carers with positive experiences of service is desirable. Data are reported by service delivery setting (residential care, admitted care and ambulatory care — see ‘Key terms and references’ tab for definitions).
In 2019-20, for jurisdictions where data are available, a higher proportion of consumers reported positive experiences of service in residential and ambulatory care (non-admitted care) than in admitted care (table 13.1).
10. Community follow-up after psychiatric admission/hospitalisation
‘Community follow-up after psychiatric admission/hospitalisation’ is an indicator of governments’ objective to provide services that are coordinated and provide continuity of care.
‘Community follow-up after psychiatric admission/hospitalisation’ is defined as the proportion of State and Territory governments’ specialised public admitted patient overnight acute separations from psychiatric units for which a community-based ambulatory contact was recorded in the seven days following separation.
A high or increasing rate of community follow-up within the first seven days of discharge from hospital is desirable.
This indicator does not measure the frequency of contacts recorded in the seven days following separation. Neither does it distinguish between the mode of contact. Only follow-up contacts made by State and Territory governments’ specialised public mental health services are included.
Nationally, the rate of community follow-up for people within the first seven days of discharge from an acute inpatient psychiatric unit was 75.1 per cent in 2019-20, an increase from 73.4 per cent in 2018-19 (figure 13.10).
Community follow-up rates by Indigenous status, remoteness areas, SEIFA, age groups and sex are in tables 13A.31-32.
11. Readmissions to hospital within 28 days of discharge
‘Readmissions to hospital within 28 days of discharge’ is an indicator of governments’ objective to provide services that are coordinated and provide continuity of care.
‘Readmissions to hospital within 28 days of discharge’ is defined as the proportion of State and Territory governments’ admitted patient overnight separations from psychiatric acute inpatient units that were followed by readmission to the same type of unit within 28 days of discharge.
A low or decreasing rate of readmissions to hospital within 28 days of discharge is desirable.
While readmissions can indicate that inpatient treatment was either incomplete or ineffective, or that follow-up care was inadequate, they can also be affected by other factors such as the cyclic and episodic nature of some illnesses.
Nationally in 2019-20, the rate of readmission to hospital acute psychiatric units within 28 days of discharge was 14.8 per cent, an increase from 14.6 per cent in 2018-19 (figure 13.11).
Data by Indigenous status, remoteness areas, SEIFA, age group and sex are in table 13A.34.
12. Workforce sustainability
‘Workforce sustainability’ is an indicator of governments’ objective to provide sustainable services.
‘Workforce sustainability’ reports age profiles for the mental health workforce. It shows the proportion of full time equivalent (FTE) medical practitioners (including psychiatrists), mental health nurses, registered psychologists and other allied mental health practitioners in ten year age brackets, by jurisdiction.
A high or increasing proportion of the workforce that has newly entered the workforce and/or a low or decreasing proportion of the workforce that is close to retirement is desirable.
These measures are not a substitute for a full workforce analysis comprising assessment of migration patterns, trends in full time work, recruitment and retention, workforce efficiency, service quality and expected demand increases. They can, however, indicate that further attention should be given to workforce sustainability for services for mental health.
Nationally in 2020, allied mental health practitioners had the highest proportion of FTEs who were aged less than 35 years, followed by nurses, psychologists and medical practitioners (including psychiatrists). The medical practitioner (including psychiatrist) workforce had the highest proportion of FTEs aged 65 years or over (figure 13.12).
13. Cost of care
‘Cost of care’ is an indicator of governments’ objective that services are delivered in an efficient manner.
‘Cost of care’ has three measures.
- ‘Cost of inpatient care’, defined by two sub measures:
- ‘Cost per inpatient bed day’, defined as expenditure on inpatient services divided by the number of inpatient bed days — data are disaggregated by hospital type (psychiatric and general hospitals) and care type (acute and non-acute units) and by inpatient target population (acute units only).
- ‘Average length of stay’, defined as the number of inpatient patient days divided by the number of separations in the reference period — data are disaggregated by inpatient target population (acute units only). Patient days for consumers who separated in the reference period (2019-20) that were admitted during the previous period (2018-19) are excluded. Patient days for consumers who remain in hospital (that is, are not included in the separations data) are included.
These sub measures are considered together for the inpatient acute units by target population to provide a ‘proxy’ measure to improve understanding of service efficiency. Average inpatient bed day costs can be reduced with longer lengths of stay because the costs of admission, discharge and more intensive treatment early in a stay are spread over more days of care. Data for forensic services are included for costs per inpatient bed day only, as the length of stay is dependent on factors outside the control of these services.
- ‘Cost of community-based residential care’ is defined as the average cost per patient day. Data are reported for both the care of adults and older people.
- ‘Cost of ambulatory care’ is defined by two sub measures:
- average cost per treatment day
- average number of treatment days per episode – this measure is provided, along with average costs, as frequency of servicing is the main driver of variation in care costs.
For each measure a low or decreasing cost per input is desirable as this might indicate more efficient service delivery. However, efficiency data need to be interpreted with care as they do not provide information on service quality or patient outcomes.
Mainstreaming has occurred at different rates across states and territories, with some jurisdictions treating a greater proportion of consumers with severe mental illnesses in community-based services than other jurisdictions (see ‘Key terms and references’ tab for a definition of mainstreaming). This can create differences across states and territories in the mix of consumers, and therefore the costs, within service types.
Nationally in 2019-20, the average cost per inpatient bed day was higher in acute than non-acute units (figure 13.13a). Older persons units have lower costs per inpatient day (table 13A.38), but have considerably longer lengths of stay than general adult or child and adolescent units (table 13A.40). Data on the average cost per inpatient bed day by target population for all care types are reported in tables 13A.38–39.
Nationally in 2019-20, the average cost for 24 hour staffed residential care is higher for general adult units ($674.19 per patient day) compared to older persons care units ($627.45 per patient day). Nationally, the cost for general adult units was just under three times the cost for those staffed 24 hours a day compared to those that were not staffed 24 hours a day (table 13A.41).
Nationally in 2019-20, the average recurrent cost per treatment day of ambulatory care was $357.15, and the average number of treatment days per episode of ambulatory care was 6.8 days (figure 13.13b).
14. Prevalence of mental illness
‘Prevalence of mental illness’ is an indicator of governments’ objective to, where possible, prevent the development of mental health problems, mental illness and suicide.
‘Prevalence of mental illness’ is defined as the proportion of the total population who have a mental illness.
A low or decreasing prevalence of mental illness can indicate that measures to prevent mental illness have been effective.
Many of the risk and protective factors that can affect the development of mental health problems and mental illness are outside the scope of the mental health system. These include environmental, sociocultural and economic factors, some of which can increase the risk of mental illness while others can support good mental health.
Not all mental illnesses are preventable and a reduction in the effect of symptoms and an improved quality of life will be a positive outcome for many people with a mental illness.
Adult prevalence data are now more than 10 years old. Nationally in 2007, the prevalence of a mental illness was 20.0 per cent for people aged 16–85 years (table 13.2), with a further 25.5 per cent reported as having a mental illness at some point in their life (table 13A.43). Data by disorder, age and sex are reported in tables 13A.43–45.
The prevalence of mental illness among children and young people aged 4–17 years was an estimated 13.9 per cent in 2013-14 (Lawrence et al. 2015). Attention deficit/hyperactivity disorder (ADHD) was the most common mental illness overall for this age group (7.4 per cent) followed by anxiety disorders (6.9 per cent) (Lawrence et al 2015).
A proxy measure of the overall mental health and wellbeing of the population is the Kessler 10 (K10) psychological distress scale. Very high levels of psychological distress may signify a need for professional help and provide an estimate of the need for mental health services (ABS 2012).
Nationally in 2017-18, the age standardised proportion of adults with high/very high levels of psychological distress was 13.0 per cent (table 13A.47), and for those with very high levels was 4.0 per cent (table 13A.46). Proportions were higher for:
- females compared to males (table 13A.46)
- people with disability compared to those without (tables 13A.47–48)
- people in lower compared to higher socioeconomic areas (tables 13A.47–48)
- Aboriginal and Torres Strait Islander people (2018-19) compared to non-Indigenous people (2017-18) (table 13A.49).
High rates of substance use and abuse can contribute to the onset of, and poor recovery from, mental illness. Information on rates of licit and illicit drug use can be found in tables 13A.50–52 and the National Drug Strategy Household Survey (AIHW 2020).
15. Mortality due to suicide
‘Mortality due to suicide’ is an indicator of governments’ objective to, where possible, prevent the development of mental health problems, mental illness and suicide.
‘Mortality due to suicide’ is defined as the suicide rate per 100 000 people. Deaths from suicide are defined as causes of death with the International Classification of Diseases (ICD) 10 codes X60–X84 and Y87.0.
A low or decreasing suicide rate per 100 000 people is desirable.
While services for mental health contribute to reducing suicides, other services also have a significant role including public mental health programs and suicide prevention programs (addressed through the initiatives of other government agencies, NGOs and other special interest groups).
Many factors outside the control of services for mental health can affect a person’s risk of suicide. These include environmental, sociocultural and economic risk factors. Often a combination of these factors can increase the risk of suicidal behaviour.
People with a mental illness are at a higher risk of suicide compared to the general population. For the period 2016–2020, 15 846 suicides were recorded in Australia — equivalent to 12.5 deaths per 100 000 people (table 13A.53). The rate for people aged 5–17 years was 2.5 deaths per 100 000 population and the rate for Aboriginal and Torres Strait Islander people was 25.6 deaths per 100 000 population (figure 13.14).
Nationally, suicide rates per 100 000 population for 2020 show that rates are lower for females compared to males (5.8 deaths compared to 18.6 deaths, ABS 2021), lower in capital cities compared to other areas (10.3 deaths compared to 15.7 deaths, table 13A.55) and (for 2015–2019) lower for non-Indigenous compared to Aboriginal and Torres Strait Islander people (12.4 deaths compared to 25.6 deaths, table 13A.56).
16. Physical health outcomes for people with a mental illness
‘Physical health outcomes for people with a mental illness’ is an indicator of governments’ objective to promote recovery and physical health and encourage meaningful participation in society.
‘Physical health outcomes for people with a mental illness’ is defined as the proportion of adults with a mental illness (compared to those without a mental illness) who experienced a long-term physical health condition: cancer, diabetes, arthritis, cardiovascular disease and asthma.
Low or decreasing proportions of people with a mental illness who experience a long-term physical health condition are desirable.
People with a mental illness have poorer physical health outcomes than people without mental illness (Happell et al. 2015; Lawrence, Hancock and Kisely 2013), but the relationship between the two is complex. Poor physical health can exacerbate mental health problems and poor mental health can lead to poor physical health. In addition, some psychiatric medications prescribed to treat mental health conditions may lead to poorer physical health.
Greater exposure to particular health risk factors can also contribute to poorer physical health. Information on selected risk factors by mental illness status can be found in table 13A.57.
A higher proportion of adults with a mental illness had long-term health conditions compared to adults without a mental illness. Nationally in 2017-18, the age standardised proportions of adults with a mental illness who had arthritis (25.9 per cent) and asthma (18.4 per cent) were higher than those without a mental illness (15.3 per cent and 9.5 per cent respectively) (figure 13.15 and table 13A.58).
17. Social and economic inclusion of people with a mental illness
‘Social and economic inclusion of people with a mental illness’ is an indicator of governments’ objective to promote recovery and physical health and encourage meaningful participation in society.
‘Social and economic inclusion of people with a mental illness’ is defined by two measures, with the proportion of people:
- aged 16–64 years with a mental illness who are employed
- aged 15 years or over with a mental illness who had face-to-face contact with family or friends living outside the household in the past week
High or increasing proportions of people with a mental illness who are employed, or who had face-to-face contact with family or friends, are desirable.
This indicator does not provide information on whether the employment, education or social activities participated in were appropriate or meaningful. It also does not provide information on why people who were not employed were not looking for work (for example, those outside the labour force).
Nationally in 2017-18, the age-standardised proportion of 16–64 year olds with a mental illness who were employed was 63.9 per cent (figure 13.16).
Information on the proportion of people aged 16–30 years with a mental illness who were employed and/or are enrolled for study in a formal secondary or tertiary qualification can be found in table 13A.59.
Nationally in 2020, the proportion of people aged 15 years or over with a mental illness who had face-to-face contact with family or friends living outside the household in the last week was 40.6 per cent (table 13.3).
18. Mental health outcomes of consumers of specialised public mental health services
‘Mental health outcomes of consumers of specialised public mental health services’ is an indicator of governments’ objective to promote recovery and physical health and encourage meaningful participation in society.
‘Mental health outcomes of consumers of specialised public mental health services’ is defined as the proportion of people receiving care who had a significant improvement in their clinical mental health outcomes, by service type. The ‘Key terms and references’ tab provides information on how the consumer outcomes average score is derived.
Outcomes are calculated for the following consumer groups:
- Group A: Consumers separated from hospital. People who received a discrete episode of inpatient care within a State/Territory designated psychiatric inpatient unit during the reference year. The defining characteristic of the group is that the episode of care commenced, and was completed, within the year.
- Group B: Consumers discharged from community‑based ambulatory care. People who received relatively short-term community care from a State/Territory mental health service during the reference year. The defining characteristic of the group is that the episode of care commenced, and was completed, within the year.
- Group C: Consumers in ongoing community‑based ambulatory care. People receiving relatively long-term community care from a State/Territory mental health service. It includes people who were receiving care for the whole of the reference year, and those who commenced community care sometime after 1 July who continued under care for the rest of the year. The defining characteristic of the group is that all remained in ongoing care when the year ended (30 June).
A high or increasing proportion of people receiving care in State and Territory governments’ specialised public mental health services who had a significant improvement in their clinical mental health outcomes is desirable.
Supplementary data are reported on the proportion of people receiving care who experienced no significant change or a significant deterioration in their mental health outcomes. Information on the proportion of episodes for which completed outcomes data are available is in table 13A.62.
This indicator has a number of issues:
- The outcome measurement tool is imprecise as a single ‘average score’ does not reflect the complex service system in which services are delivered across multiple settings and provided as both discrete, short-term episodes of care and prolonged care over indefinite periods (AHMC 2012).
- The approach separates a consumer’s care into segments (hospital versus the community) rather than tracking his or her overall outcome across treatment settings.
- Consumers’ outcomes are measured from the clinician’s perspective rather than the consumer’s.
Nationally in 2019-20, 72.2 per cent of people discharged from a hospital psychiatric inpatient unit, 50.7 per cent of people discharged from community-based ambulatory care and 27.1 per cent of people in ongoing community-based ambulatory care showed a significant improvement in their clinical mental health outcomes (figure 13.17).
Over the 10 years of data in this Report, for those in ongoing community-based ambulatory care, younger people aged 0–17 years had the highest proportion of people who showed a significant improvement compared to other age groups (table 13A.63).
19. Stigma and discrimination experienced by people living with mental health problems or mental illness
‘Stigma and discrimination experienced by people living with mental health problems or mental illness’ is an indicator of governments’ objective to reduce the impact of mental illness (including the effects of stigma and discrimination).
‘Stigma and discrimination experienced by people with a mental health condition’ is defined by two measures:
- the proportion of people with a mental health condition who have experienced discrimination or been treated unfairly
- the proportion of people with a mental health condition who have experienced discrimination or been treated unfairly because of their mental health condition.
A low or decreasing proportion of people experiencing discrimination or being treated unfairly is desirable.
In 2020, 20.8 per cent of people with a mental illness reported having experienced discrimination or been treated unfairly (table 13.4). Data are not available on whether the discrimination was perceived to be due to a person’s mental illness.
Performance indicator data for Aboriginal and Torres Strait Islander people in this section are available in the data tables listed below. Further supporting information can be found in the 'Indicator results' tab and data tables.
| Table number | Table title |
|---|---|
| Table 13A.17 | Proportion of people receiving clinical mental health services by service type and Indigenous status |
| Table 13A.22 | Proportion of young people (aged < 25 years) who had contact with MBS subsidised primary mental health care services, by selected characteristics (per cent) |
| Table 13A.31 | Rates of community follow up within first seven days of discharge from a psychiatric admission, by State and Territory, by Indigenous status and remoteness |
| Table 13A.34 | Readmissions to hospital within 28 days of discharge, by selected characteristics |
| Table 13A.49 | Age-standardised rate of adults with high/ very high levels of psychological distress, by State and Territory, by Indigenous status |
| Table 13A.56 | Suicide deaths, by Indigenous status |
Key terms
| Terms | Definition |
|---|---|
Accrued mental health patient days | Mental health care days are days of admitted patient care provided to admitted patients in psychiatric hospitals, designated psychiatric units and days of residential care provided to residents in residential mental health services. Accrued mental health patient days can also be referred to as occupied bed days in specialised mental health services. The days to be counted are only those days occurring within the reference period, which is from 1 July to the following 30 June for the relevant period, even if the patient/resident was admitted prior to the reference period or discharged after the reference period. In short, the number of accrued mental health care days are calculated as follows:
|
Admitted care | A specialised mental health service that provides overnight care in a psychiatric hospital or a specialised mental health unit in an acute hospital. Psychiatric hospitals and specialised mental health units in acute hospitals are establishments devoted primarily to the treatment and care of admitted patients with psychiatric, mental or behavioural disorders. These services are staffed by health professionals with specialist mental health qualifications or training and have as their principal function the treatment and care of patients affected by mental disorder/illness. |
Acute services | Services that primarily provide specialised psychiatric care for people with acute episodes of mental illness. These episodes are characterised by recent onset of severe clinical symptoms of mental illness that have potential for prolonged dysfunction or risk to self and/or others. The key characteristic of acute services is that the treatment effort focuses on symptom reduction with a reasonable expectation of substantial improvement. In general, acute psychiatric services provide relatively short-term treatment. Acute services can:
|
Ambulatory care | A specialised mental health service that provides services to people who are not currently admitted to a mental health admitted or residential service. Services are delivered by health professionals with specialist mental health qualifications or training. Ambulatory mental health services include:
|
Anxiety disorders | Feelings of tension, distress or nervousness. Includes agoraphobia, social phobia, panic disorder, generalised anxiety disorder, obsessive-compulsive disorder and post‑traumatic stress disorder. |
Carer staff | A person specifically employed for the expertise developed from their experience as a mental health carer. |
Child and adolescent services | These services principally target children and young people under the age of 18 years. The classification of a service into this category requires recognition by the regional or central funding authority of the special focus of the service. These services may include a forensic component. |
Community‑based residential care | Staffed residential units established in community settings that provide specialised treatment, rehabilitation or care on an overnight basis in a domestic‑like environment for people affected by a mental illness or psychiatric disability. To be defined as community‑based residences, services must: provide residential care to people with mental illnesses or psychiatric disability; be located in a community setting external to the campus of a general hospital or psychiatric institution; employ onsite staff for at least some part of the day; and be government funded. |
Comparability | Data are considered comparable if (subject to caveats) they can be used to inform an assessment of comparative performance. Typically, data are considered comparable when they are collected in the same way and in accordance with the same definitions. For comparable indicators or measures, significant differences in reported results allow an assessment of differences in performance, rather than being the result of anomalies in the data. |
Completeness | Data are considered complete if all required data are available for all jurisdictions that provide the service. |
Consumer staff | A person specifically employed for the expertise developed from their lived experience of mental illness. |
Forensic mental health services | Services principally providing assessment, treatment and care of mentally ill people whose behaviour has led them to commit criminal offences or makes it likely that they will offend in the future if not adequately treated and contained. This includes prison‑based services but excludes services that are primarily for children and adolescents and for older people even where they include a forensic component. |
General mental health services | Services that principally target the general adult population (18‑65 years old) but that can provide services to children, adolescents or older people. Includes, therefore, services that cannot be described as specialised child and adolescent services, youth services, services for older people or forensic services. General mental health services include hospital units with a principal function to provide some form of specialised service to the general adult population (for example, inpatient psychotherapy) or to focus on specific clinical disorders within the adult population (for example, postnatal depression, anxiety disorders). |
General practice | The organisational structure in which one or more GPs provide and supervise health care for a ‘population’ of patients. |
Health management | The ongoing process beginning with initial consumer contact and including all actions relating to the consumer. Includes assessment/evaluation, education of the person, family or carer(s), and diagnosis and treatment. Involves problems with adherence to treatment and liaison with, or referral to, other agencies. |
Mainstreaming | The First National Mental Health Plan emphasised decreasing the number of psychiatric beds in favour of community‑based options, reducing the reliance on stand‑alone psychiatric hospitals, and ‘mainstreaming’ the delivery of acute inpatient care into general hospitals. |
Mental health | The capacity of individuals within groups and the environment to interact with one another in ways that promote subjective wellbeing, the optimal development and use of mental abilities (cognitive, affective and relational) and the achievement of individual and collective goals consistent with justice. |
Mental health problems | Diminished cognitive, emotional or social abilities, but not to the extent of meeting the criteria for a mental illness. |
Mental illness | A diagnosable illness that significantly interferes with an individual’s cognitive, emotional and/or social abilities. |
National Standards for Mental Health Services (NSMHS) | Services at level 1 — services reviewed by an external accreditation agency and judged to have met all National Standards. Services at level 2 — services reviewed by an external accreditation agency and judged to have met some but not all National Standards. Services at level 3 — services (i) in the process of being reviewed by an external accreditation agency but the outcomes are not known, or (ii) booked for review by an external accreditation agency. Services at level 4 — services that do not meet criteria detailed under levels 1 to 3 (AHMC 2010). |
Non‑acute services | Non-acute services are defined by two categories:
|
Non‑government organisations (NGOs) | Private not-for-profit community managed organisations that receive government funding specifically for the purpose of providing community support services for people affected by a mental illness or psychiatric disability. Programs provided by the NGO sector can include supported accommodation services (including community‑based crisis and respite beds), vocational rehabilitation programs, advocacy programs (including system advocacy), consumer self‑help services, and support services for families and primary carers. |
Older persons mental health services | Services principally targeting people in the age group 65 years or over. Classification of services in this category requires recognition by the regional or central funding authority of the special focus of the inpatient service on aged people. These services can include a forensic component. Excludes general mental health services that may treat older people as part of a more general service. |
Outcomes measurement — calculating the consumers ‘score’. | The assessment of a consumer’s clinical mental health outcomes is based on the changes reported in a consumer’s ‘score’ on a rating scale known as the Health of the Nation Outcomes Scale (HoNOS), or for children and adolescents, the Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). Outcome scores are classified based on effect size — a statistic used to assess the magnitude of a treatment effect (AHMC 2012). The effect size is based on the ratio of the difference between the pre and post scores to the standard deviation of the pre score. Individual episodes are classified as ‘significant improvement’ if the effect size index is greater than or equal to positive 0.5; ‘no change’ if the index is between 0.5 and ‑0.5; and ‘significant deterioration’ if the effect size index is less than or equal to ‑0.5 (AHMC 2012). |
Outpatient services — community‑based | Services primarily provided to non‑admitted patients on an appointment basis and delivered from health centres located in community settings, physically separated within hospital sites. They can include outreach or domiciliary care as an adjunct to services provided from the centre base. |
Outpatient services — hospital based | Services primarily provided to non‑admitted patients on an appointment basis and delivered from clinics located within hospitals. They can include outreach or domiciliary care as an adjunct to services provided from the clinic base. |
Prevalence | The number of cases of a disease present in a population at a given time (point prevalence) or during a given period (period prevalence). |
Preventive interventions | Programs designed to decrease the incidence, prevalence and negative outcomes of illnesses. |
Psychiatric hospitals | Health establishments that are primarily devoted to the treatment and care of inpatients with psychiatric, mental or behavioural disorders, and that are situated at physically separate locations from a general hospital. Stand‑alone hospitals may or may not be managed by the mainstream health system. Psychiatric hospitals situated at physically separate locations from a general hospital are included within the ‘stand‑alone’ category regardless of whether they are under the management control of a general hospital. A health establishment that operates in a separate building but is located on, or immediately adjoining, the acute care hospital campus can also be a stand‑alone hospitals if the following criteria are not met:
|
Psychiatrist | A medical practitioner with specialist training in psychiatry. |
Public health | The organised, social response to protect and promote health, and to prevent illness, injury and disability. The starting point for identifying public health issues, problems and priorities, and for designing and implementing interventions, is the population as a whole or population subgroups. Public health is characterised by a focus on the health of the population (and particular at-risk groups) and complements clinical provision of health care services. |
Public (non‑psychiatric) hospital | A hospital that provides at least minimum medical, surgical or obstetric services for inpatient treatment and/or care, and around the clock, comprehensive, qualified nursing services, as well as other necessary professional services. |
Restraint | Mechanical restraint: The application of devices (including belts, harnesses, manacles, sheets and straps) on a person’s body to restrict his or her movement. This is to prevent the person from harming himself/herself or endangering others or to ensure the provision of essential medical treatment. It does not include the use of furniture (including beds with cot sides and chairs with tables fitted on their arms) that restricts the person’s capacity to get off the furniture except where the devices are used solely for the purpose of restraining a person’s freedom of movement. The use of a medical or surgical appliance for the proper treatment of physical disorder or injury is not considered mechanical restraint. Physical restraint: The application by health care staff of hands‑on immobilisation or the physical restriction of a person to prevent the person from harming himself/herself or endangering others or to ensure the provision of essential medical treatment. |
Schizophrenia | A combination of signs and symptoms that can include delusions, hallucinations, disorganised speech or behaviour, a flattening in emotions, and restrictions in thought, speech and goal directed behaviour. |
Seclusion | Seclusion is the confinement of the consumer at any time of the day or night alone in a room or area from which free exit is prevented. The intended purpose of the confinement is not relevant in determining what is or is not seclusion. Seclusion applies even if the consumer agrees or requests the confinement (NMHPSC 2011b). The awareness of the consumer that they are confined alone and denied exit is not relevant in determining what is or is not seclusion. The structure and dimensions of the area to which the consumer is confined is not relevant in determining what is or is not seclusion. The area may be an open area, for example, a courtyard. Seclusion does not include confinement of consumers to High Dependency sections of gazetted mental health units, unless it meets the definition (AIHW 2015). |
Seclusion event | An event is when a consumer enters seclusion and when there is a clinical decision to cease seclusion. Following the clinical decision to cease seclusion, if a consumer re‑enters seclusion within a short period of time this would be considered a new seclusion event. The term ‘seclusion event’ is utilised to differentiate it from the different definitions of ‘seclusion episode’ used across jurisdictions (NMHPSC 2011b). |
Separation | Separation is the process by which an episode of care for an admitted patient is completed. A separation may be formal or statistical. An episode of care may be completed because the patient’s treatment is complete, the patient no longer requires care, has deceased, is transferred to another hospital/care facility or the patient leaves the hospital against medical advice. |
Specialised mental health inpatient services | Services provided to admitted patients in stand‑alone psychiatric hospitals or specialised psychiatric units located within general hospitals. |
Specialised mental health services | Services whose primary function is specifically to provide treatment, rehabilitation or community support targeted towards people affected by a mental illness or psychiatric disability. Further, such activities are delivered from a service or facility that is readily identifiable as both specialised and serving a mental health function. This criterion applies regardless of the source of funds. |
Specialised residential mental health services | Services provided in the community that are staffed by mental health professionals on a non 24 or 24 hour basis. |
Staffing categories (mental health) | Medical officers: all medical officers employed or engaged by the organisation on a full time or part time basis. Includes visiting medical officers who are engaged on an hourly, sessional or fee for service basis. Psychiatrists and consultant psychiatrists: medical officers who are registered to practice psychiatry under the relevant State or Territory medical registration board; or who are fellows of the Royal Australian and New Zealand College of Psychiatrists or registered with Health Insurance Commission as a specialist in Psychiatry. Psychiatry registrars and trainees: medical officers who are formal trainees within the Royal Australian and New Zealand College of Psychiatrists’ Postgraduate Training Program. Other medical officers: medical officers employed or engaged by the organisation who are not registered as psychiatrists within the State or Territory, or as formal trainees within the Royal Australian and New Zealand College of Psychiatrists’ Postgraduate Training Program. Nursing staff: all categories of registered nurses and enrolled nurses, employed or engaged by the organisation. Registered nurses: people with at least a three-year training certificate or tertiary qualification who are certified as being a registered nurse with the State or Territory registration board. This is a comprehensive category and includes general and specialised categories of registered nurses. Enrolled nurses: refers to people who are second level nurses who are enrolled in all states except Victoria where they are registered by the State registration board to practise in this capacity. Includes general enrolled nurse and specialist enrolled nurse (e.g. mothercraft nurses in some states). Diagnostic and health professionals (allied health professionals): qualified staff (other than qualified medical or nursing staff) who are engaged in duties of a diagnostic, professional or technical nature. This category covers all allied health professionals, such as social workers, psychologists, occupational therapists, physiotherapists, and other diagnostic and health professionals. Social workers: people who have completed recognised training and are eligible for membership of the Australian Association of Social Workers. Psychologists: people who are registered as psychologists with the relevant State or Territory registration board. Occupational therapists: people who have completed a course of recognised training and who are eligible for membership of the Australian Association of Occupational Therapists. Other personal care staff: attendants, assistants, home companions, family aides, ward helpers, warders, orderlies, ward assistants and nursing assistants who are engaged primarily in the provision of personal care to patients or residents, and who are not formally qualified or who are undergoing training in nursing or allied health professions. Administrative and clerical staff: staff engaged in administrative and clerical duties. Excludes medical, nursing, diagnostic and health professional and domestic staff wholly or partly involved in administrative and clerical duties, who should be counted under their appropriate occupational categories. Civil engineers and computing staff are included in this category. Domestic and other staff: staff involved in the provision of food and cleaning services including domestic staff primarily engaged in administrative duties such as food services manager. Dieticians are excluded. |
Substance use disorders | Disorders in which drugs or alcohol are used to such an extent that behaviour becomes maladaptive, social and occupational functioning is impaired, and control or abstinence becomes impossible. Reliance on the drug can be psychological (as in substance misuse) or physiological (as in substance dependence). |
Youth mental health services | Services principally targeting children and young people generally aged 16‑24 years. The classification of a service into this category requires recognition by the regional or central funding authority of the special focus of the service. These services may include a forensic component. |
References
ABS (Australian Bureau of Statistics) 2021, Causes of Death, Australia, 2020 https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/2020 (accessed 14 October 2021).
—— 2012, Information Paper: Use of the Kessler Psychological Distress Scale in ABS Health Surveys, Australia, 2007-08, Cat. no. 4817.0.55.001, Canberra.
Australian Health Ministers 1991, Mental Health Statement of Rights and Responsibilities, Australian Government Publishing Service, Canberra.
AHMC (Australian Health Ministers’ Conference) 2010, National Standards for Mental Health Services 2010, Canberra.
—— 2012, Council of Australian Governments National Action Plan for Mental Health 2006–2011: Progress Report 2009-10, Report prepared under the auspice of the Mental Health Standing Committee of the Australian Health Ministers’ Advisory Council.
AIHW (Australian Institute of Health and Welfare) 2021, Mental Health Services in Australia Online, https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/summary (accessed 14 October 2021).
—— 2020, National Drug Strategy Household Survey detailed report 2019, Drug statistics series no. 32, Cat. no. PHE 270, Canberra.
—— 2015, Seclusion, Meteor Metadata Online Registry, http://meteor.aihw.gov.au/content/index.phtml/itemId/557975 (accessed 18 December 2017).
COAG (Council of Australian Governments) 2017, The Fifth National Mental Health and Suicide Prevention Plan (the Fifth Plan), https://apo.org.au/system/files/114356/apo-nid114356-451131.pdf (accessed 18 October 2018).
DoH (Department of Health) 2014, National mental health strategy, https://www1.health.gov.au/internet/main/publishing.nsf/Content/mental-strat (accessed 17 December 2019).
—— 2009, National mental health policy 2008, https://www1.health.gov.au/internet/main/publishing.nsf/Content/mental-pubs-n-pol08 (accessed 16 October 2019).
DHAC (Australian Government Department of Health and Community Services) and AIHW 1999, National Health Priority Areas Report: Mental Health 1998, AIHW Cat. no. PHE 13, Canberra.
Happell, B., Platania Phung, C., Webster, S., McKenna, B., Millar, F., Stanton, R., Galletly, C., Castle, D., Furness, T., Liu, D. and Scott, D 2015, ‘Applying the World Health Organization Mental Health Action Plan to evaluate policy on addressing co-occurrence of physical and mental illnesses in Australia’, Australian Health Review, Vol. 39, pp. 370–378, CSIRO Publishing (available at http://dx.doi.org/10.1071/AH14098).
Lawrence, D., Hancock, K. and Kisely S. 2013, ‘The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers’, British Medical Journal, Vol. 346.
Lawrence, D., Johnson, S., Hafekost, J., Boterhoven, K., Sawyer, M., Ainley, J., Zubrick, S. 2015, The Mental Health of Children and Adolescents. Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing, Department of Health, Canberra.
NDIA (National Disability Insurance Agency) 2021, Public Data Sharing platform (NDIS Public Data), https://data.ndis.gov.au/explore-data (accessed 10 October 2021).
NMHPSC (National Mental Health Performance Subcommittee) 2011a, The Fourth National Mental Health Plan Measurement Strategy 2011, Report produced for the Australian Health Ministers Advisory Council Mental Health Standing Committee, https://www.aihw.gov.au/getmedia/d8e52c84-a53f-4eef-a7e6-f81a5af94764/Fourth-national-mental-health-plan-measurement-strategy-2011.pdf.aspx (accessed 17 December 2019).
—— 2011b, Key performance indicators for Australian public mental health services: second edition 2011, Report produced for the Australian Health Ministers Advisory Council Mental Health Standing Committee, https://www.aihw.gov.au/getmedia/3c6614bb-87fd-4328-b276-f69542082a7c/Key-performance-indicators-for-Australian-public-mental-health-services-second-edition-2011.pdf.aspx (accessed 17 December 2019).
RACGP (Royal Australian College of General Practitioners) 2019, General Practice: Health of the Nation 2019, East Melbourne, Victoria.
WHO (World Health Organization) 2001, Strengthening mental health promotion, Fact sheet no. 220, Geneva.
Download supporting material
- 13 Services for mental health data tables (XLSX - 615 Kb)
- 13 Services for mental health dataset (CSV - 1775 Kb)
See the corresponding table number in the data tables for detailed definitions, caveats, footnotes and data source(s).