Report on Government Services 2020
PART E, SECTION 13: PRESENTATION REVISED ON 25 JUNE 2020
13 Mental health management
The presentation of this section has been updated since its release on 31 January 2020. To access material in the original format please refer to the archived copy
This section is presented in a new online format. Dynamic data visualisations replace the static chapter format used in previous editions. Machine readable data are also available for download. A guide is available on accessing information in the new format.
This section reports on the Australian, State and Territory governments’ management of mental health and mental illnesses. Performance reporting focuses on State and Territory governments’ specialised mental health services, and mental health services subsidised under the Medicare Benefits Schedule (MBS) (provided by General Practitioners (GPs), psychiatrists, psychologists and other allied health professionals).
The Indicator Results tab uses data from the data tables to provide information on the performance for each indicator in the Indicator Framework. The same data are also available in CSV format.
Skip to downloadable Mental health management data tables and supporting material
- Context
- Indicator Framework
- Indicator Results
- Indigenous Data
Objectives for mental health services
Mental health services aim to:
- promote mental health and wellbeing, and where possible prevent the development of mental health problems, mental illness and suicide, and
- when mental health problems and illness do occur, reduce the impact (including the effects of stigma and discrimination), promote recovery and physical health and encourage meaningful participation in society, by providing services that:
- are high quality, safe and responsive to consumer and carer goals
- facilitate early detection of mental health issues and mental illness, followed by appropriate intervention
- are coordinated and provide continuity of care
- are timely, affordable and readily available to those who need them
- are sustainable.
Governments aim for mental health services to meet these objectives in an equitable and efficient manner.
Service overview
Mental health relates to an individual’s ability to negotiate the daily challenges and social interactions of life without experiencing undue emotional or behavioural incapacity (DHAC 1999). The World Health Organization describes positive mental health as:
… a state of well‑being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community (WHO 2001).
Mental illness is a term that describes a diverse range of behavioural and psychological conditions. These conditions can affect an individual’s mental health, functioning and quality of life. Each mental illness is unique in its incidence across the lifespan, causal factors and treatments.
There are a range of services provided or funded by Australian, State and Territory governments that are specifically designed to meet the needs of people with mental health issues; the key services are:
- MBS subsidised mental health specific services that are partially or fully funded under Medicare on a fee-for-service basis and are provided by GPs, psychiatrists, psychologists or other allied health professionals under specific mental health items.
- State and Territory government specialised mental health services (treating mostly low prevalence, but severe, mental illnesses), which include:
- Admitted patient care in public hospitals — specialised services provided to inpatients in stand-alone psychiatric hospitals or psychiatric units in general acute hospitals1.
- Community-based public mental health services, comprising:
- ambulatory care services and other services dedicated to assessment, treatment, rehabilitation and care, and
- residential services that provide beds in the community, staffed onsite by mental health professionals.
- Not for profit, non-government organisation (NGO) services, funded by the Australian, State and Territory governments focused on providing well-being, support and assistance to people who live with a mental illness.
- The National Disability Insurance Scheme (NDIS), which began full roll out in July 20162. People with a psychiatric disability who have significant and permanent functional impairment are eligible to access funding through the NDIS. In addition, people with a disability other than a psychiatric disability, may also be eligible for funding for mental health-related services and support if required.
- Whilst not a State and Territory government specialised mental health service, this section also reports on emergency department presentations for mental health related care needs (where data are available). Locate Footnote 1 above
- For further information on the NDIS and its implementation see https://www.ndis.gov.au/. Locate Footnote 2 above
Roles and responsibilities
State and Territory governments are responsible for the funding, delivery and/or management of specialised mental health services including inpatient/admitted care in hospitals, community-based ambulatory care and community-based residential care.
The Australian Government is responsible for the oversight and funding of a range of mental health services and programs that are primarily provided or delivered by private practitioners or NGOs. These services and programs include MBS subsidised services provided by GPs (under both general and specific mental health items), private psychiatrists and other allied mental health professionals, Pharmaceutical Benefits Scheme (PBS) funded mental health related medications and other programs designed to prevent suicide or increase the level of social support and community-based care for people with a mental illness and their carers. The Australian Government also funds State and Territory governments for health services, most recently through the approaches specified in the National Health Reform Agreement (NHRA) which includes a mental health component.
A number of national initiatives and nationally agreed strategies and plans underpin the delivery and monitoring of mental health services in Australia including:
- the Mental Health Statement of Rights and Responsibilities (Australian Health Ministers 1991)
- the National Mental Health Policy 2008 (DoH 2009)
- the National Mental Health Strategy (DoH 2014)
- five-yearly National Mental Health Plans, with the most recent ― the Fifth National Mental Health and Suicide Prevention Plan — endorsed in August 2017 (COAG 2017).
Funding
Nationally, real government recurrent expenditure of around $9.4 billion was allocated to mental health services in 2017‑18, equivalent to $377.79 per person in the population (table 13A.1 and figure 13.1). State and Territory governments made the largest contribution ($6.0 billion or 64.1 per cent, which includes Australian Government funding under the NHRA), with Australian Government expenditure of $3.4 billion (table 13A.1).
Expenditure on MBS subsidised services was the largest component of Australian Government expenditure on mental health services in 2017‑18 ($1.2 billion or 37.0 per cent) (table 13A.2). This comprised MBS payments for psychologists and other allied health professionals (17.4 per cent), consultant psychiatrists (10.7 per cent) and GP services (8.9 per cent) (table 13A.2). Another significant area of Australian Government expenditure on mental health services in 2017‑18 was expenditure under the PBS for mental health related medications ($519.9 million) (table 13A.2).
Nationally, expenditure on admitted patient services is the largest component of State and Territory governments’ expenditure on specialised mental health services ($2.6 billion or 43.7 per cent) in 2017‑18 followed by expenditure on community-based ambulatory services ($2.3 billion or 37.3 per cent) (table 13A.3). State and Territory governments’ expenditure on specialised mental health services, by source of funds and depreciation (which is excluded from reporting) are in tables 13A.4 and 13A.5 respectively.
Size and scope
In 2017‑18, 1.9 per cent and 10.6 per cent of the total population received State and Territory governments’ specialised mental health services and MBS/Department of Veterans’ Affairs (DVA) services, respectively (figure 13.2). While the proportion of the population using State and Territory governments’ specialised mental health services has remained relatively constant, the proportion using MBS/DVA services has increased steadily over time from 5.9 per cent in 2008‑09 to 10.6 per cent in 2017‑18 (table 13A.7). Much of this growth has come from greater utilisation of GP mental health-specific services (from 4.4 per cent to 8.7 per cent) and other allied health services (1.7 per cent to 3.3 per cent) over that period (table 13A.7).
Information on the proportion of new consumers who accessed State and Territory governments’ specialised and MBS subsidised mental health services are available in tables 13A.8–9.
MBS subsidised mental health services
In 2017‑18, 8.0 million MBS subsidised mental health services were provided by; psychologists (5.2 million), psychiatrists (2.4 million) and other allied health professionals (0.4 million). Service usage rates varied across states and territories (table 13A.10).
A further 3.6 million MBS subsidised specific mental health services were provided by GPs (table 13A.10). GPs are often the first service accessed by people seeking help when suffering from a mental illness (AIHW 2019). They can diagnose, manage and treat mental illnesses and refer patients to more specialised service providers. A recent report from the Royal Australian College of General Practitioners found that mental health issues are the most common single reason patients are visiting their GP (RACGP 2019). Data from the now decommissioned Bettering the Evaluation and Care of Health (BEACH) survey of general practice activity showed an estimated 18.0 million GP visits in 2016‑17 included management of mental health related problems (12.4 per cent of all GP encounters) (table 13A.11).State and Territory governments’ specialised mental health services
Across states and territories, the mix of admitted patient and community-based services and care types can differ. As the unit of activity varies across these three service types, service mix differences can be partly understood by considering items which have comparable measurement such as expenditure (table 13A.3), numbers of full time equivalent (FTE) direct care staff (table 13A.12), accrued mental health patient days (table 13A.13) and mental health beds (table 13A.14).
Additional data are also available on the most common principal diagnosis for admitted patients, community-based ambulatory contacts by age group and specialised mental health care by Indigenous status in Mental Health Services in Australia (AIHW 2019).
National Disability Insurance Scheme
By 2019‑20, the number of participants in the NDIS with a significant and enduring primary psychosocial disability is estimated to be approximately 64 000 (NDIA 2017). In 2018‑19, there were 25 192 NDIS participants (active with an approved plan) with a psychosocial disability (9 per cent of all participants) (NDIA 2019).
Nationally in 2018‑19, payments for active participants (with an approved plan) for people with a primary disability of psychosocial disability totalled $550.8 million (table 13A.15).
References
ABS (Australian Bureau of Statistics), 2019, Causes of Death, Australia, 2018, Cat. no. 3303.0, Canberra.
—— 2012, Information Paper: Use of the Kessler Psychological Distress Scale in ABS Health Surveys , Australia, 2007‑08, Cat. no. 4817.0.55.001, Canberra.
Australian Health Ministers 1991, Mental Health Statement of Rights and Responsibilities , Australian Government Publishing Service, Canberra.
AIHW (Australian Institute of Health and Welfare) 2017, National Drug Strategy Household Survey detailed report 2016 , Drug statistics series no. 31, Cat. no. PHE 214, Canberra.
—— 2019, Mental Health Services in Australia Online , https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/summary (accessed 11 December 2019).
COAG (Council of Australian Governments) 2017, The Fifth National Mental Health and Suicide Prevention Plan (the Fifth Plan) , apo.org.au/system/files/114356/apo-nid114356-451131.pdf (accessed 18 October 2018).
DoH (Department of Health) 2014, National mental health strategy , https://www1.health.gov.au/internet/main/publishing.nsf/Content/mental-strat (accessed 17 December 2019).
—— 2009, National mental health policy 2008 , https://www1.health.gov.au/internet/main/publishing.nsf/Content/mental-pubs-n-pol08 (accessed 16 October 2019).
DHAC (Australian Government Department of Health and Community Services) and AIHW 1999, National Health Priority Areas Report: Mental Health 1998 , AIHW Cat. no. PHE 13, Canberra.
Lawrence, D., Johnson, S., Hafekost, J., Boterhoven, K., Sawyer, M., Ainley, J., Zubrick, S. 2015, The Mental Health of Children and Adolescents. Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing , Department of Health, Canberra.
NDIA (National Disability Insurance Agency) 2017, Key Data on Psychosocial Disability and the NDIS - as at 31 December 2017 , https://www.ndis.gov.au (accessed 4 October 2018).
—— 2019, COAG Disability Reform Council Quarterly Report 30 June 2019 , https://www.ndis.gov.au/media/1611/download (accessed 17 December 2019).
RACGP (Royal Australian College of General Practitioners) 2019, General Practice: Health of the Nation 2019 . East Melbourne, Victoria.
WHO (World Health Organization) 2001, Strengthening mental health promotion , Fact sheet no. 220, Geneva.
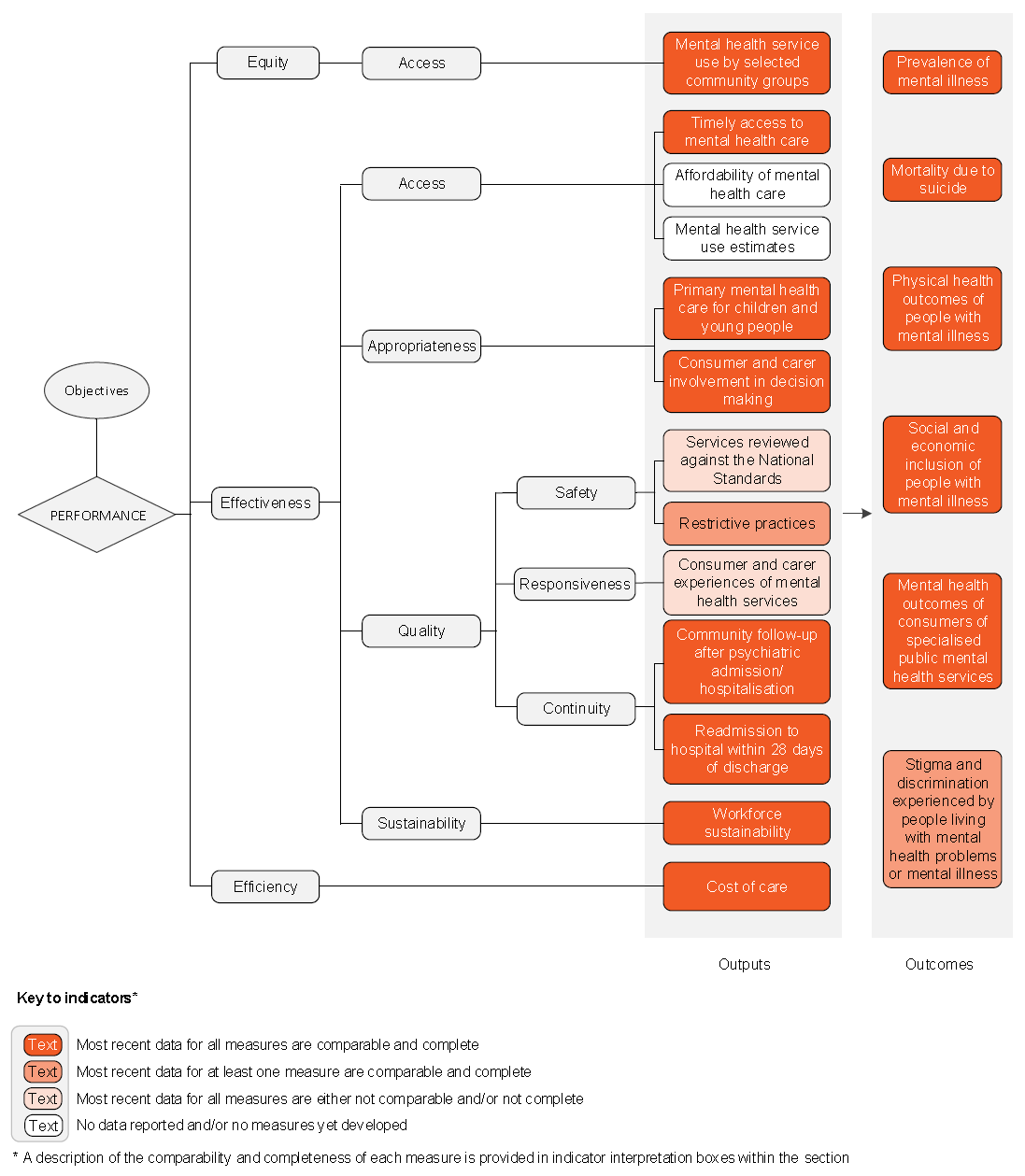
The performance indicator framework provides information on equity, efficiency and effectiveness, and distinguishes the outputs and outcomes of mental health services.
The performance indicator framework shows which data are complete and comparable in this Report. For data that are not considered directly comparable, text includes relevant caveats and supporting commentary. Section 1 discusses data comparability and completeness from a Report-wide perspective. In addition to the service area's Profile information, the Report’s statistical context (section 2) contains data that may assist in interpreting the performance indicators presented in this section.
Improvements to performance reporting for mental health services are ongoing and include identifying data sources to fill gaps in reporting for performance indicators and measures, and improving the comparability and completeness of data.
Outputs
Outputs are the services delivered (while outcomes are the impact of these services on the status of an individual or group) (see section 1). Output information is also critical for equitable, efficient and effective management of government services.
Outcomes
Outcomes are the impact of services on the status of an individual or group (see section 1).
An overview of the mental health services performance indicator results are presented. Different delivery contexts, locations and types of consumers can affect the equity, effectiveness and efficiency of mental health services.
Information to assist the interpretation of these data can be found in the mental health services supporting interpretative material and data tables. Data tables are identified by a ‘13A’ prefix (for example, table 13A.1).
All data are available for download as an excel spreadsheet and as a CSV dataset — refer to Download supporting material. Specific data used in figures can be downloaded by clicking in the figure area, navigating to the bottom of the visualisation to the grey toolbar, clicking on the 'Download' icon and selecting 'Data' from the menu. Selecting 'PDF' or 'Powerpoint' from the 'Download' menu will download a static view of the performance indicator results.
Performance indicator data for Aboriginal and Torres Strait Islander people in this section are available in the data tables listed below. Contextual data and further supporting information can be found in the section.
| Table number | Table title |
|---|---|
| Table 13A.17 | Proportion of people receiving clinical mental health services by service type and Indigenous status |
| Table 13A.21 | Proportion of young people (aged < 25 years) who had contact with MBS subsidised primary mental health care services, by selected characteristics (per cent) |
| Table 13A.30 | Rates of community follow up within first seven days of discharge from a psychiatric admission, by State and Territory, by Indigenous status and remoteness |
| Table 13A.33 | Readmissions to hospital within 28 days of discharge, by selected characteristics |
| Table 13A.48 | Age-standardised rate of adults with high/ very high levels of psychological distress, by State and Territory, by Indigenous status |
| Table 13A.55 | Suicide deaths, by Indigenous status |
Download supporting material
- 13 Mental health management interpretative material (PDF - 850 Kb)
- 13 Mental health management interpretative material (Word - 60 Kb)
- 13 Mental health management data tables (XLSX - 1907 Kb)
- 13 Mental health management dataset (CSV - 1897 Kb)
See the interpretative material and corresponding table number in the data tables for detailed definitions, caveats, footnotes and data source(s).
Note: an errata was released for section 13 Mental health services.
Errata
The following data have changed for section 13 Mental health data tables:
- Table 13A.11: Amended year labels for all years.
- Table 13A.37: Amended data for general mental health services for 2008-09 to 2011-12 for the ACT, NT and Australia; Child and adolescent mental health services for 2008-09 to 2011-12 for Vic, SA and Australia; Older persons mental health services for 2008-09 to 2011-12 for Vic, ACT and Australia; Forensic mental health services for 2008-09 to 2011-12 for Queensland, Tasmania and Australia.
- Table 13A.38: Amended data for acute forensic mental health services for the period of 2008-09 for Australia.
- Table 13A.61: Amended data for group A and group C proportions for the period of 2008-09 for all jurisdictions.